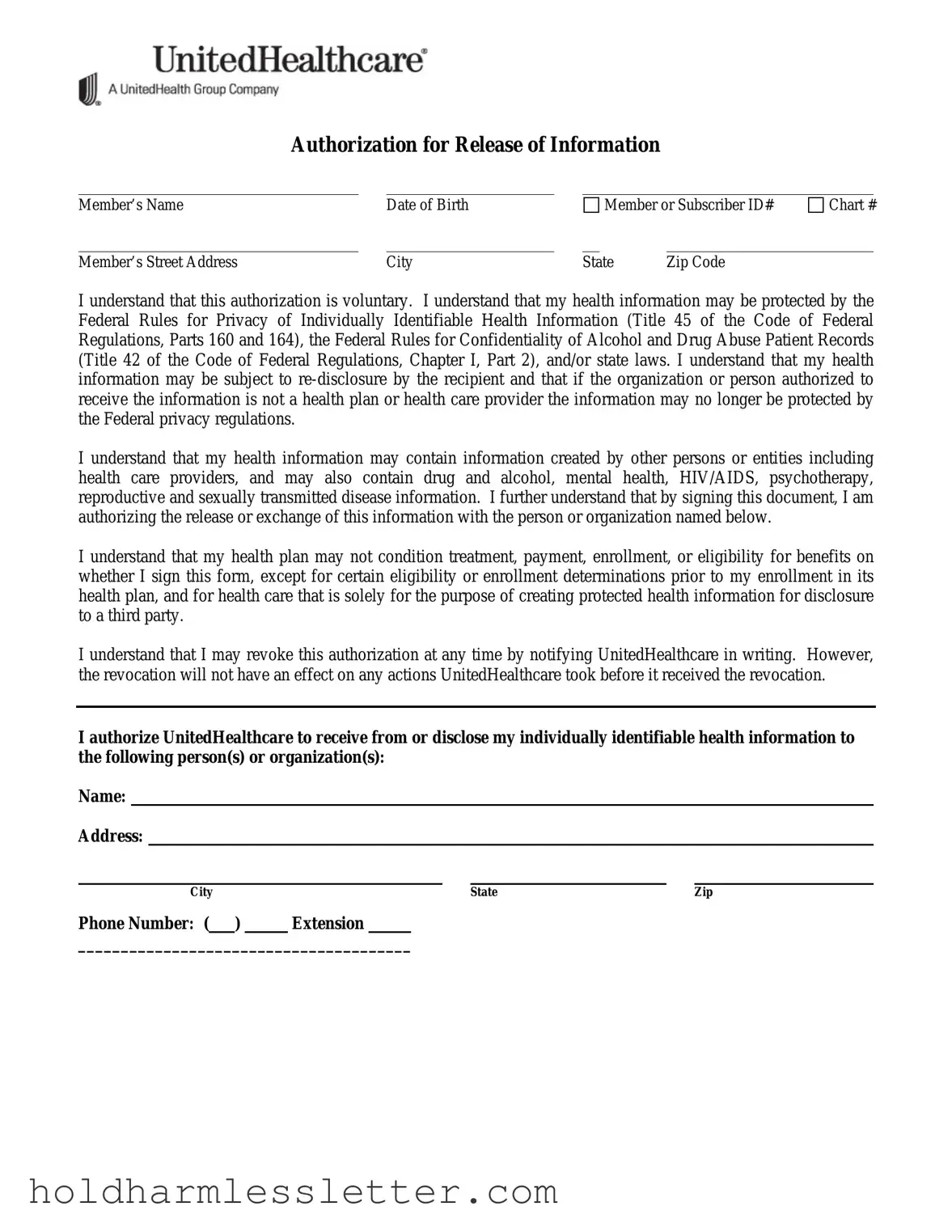
What is the United Healthcare Release of Information form used for?
The United Healthcare Release of Information form is a document that allows the disclosure of personal health information by UnitedHealthcare to designated persons or organizations, or from designated persons or organizations to UnitedHealthcare. This can include information such as treatment plans, claims information, attendance records, eligibility benefits, and more. It is commonly used for purposes like managing treatment and services, benefit administration, claims administration/payment, and compliance with legal processes.
Is signing the United Healthcare Release of Information form mandatory for receiving treatment or benefits?
No, signing this form is voluntary. Your decision to sign or not sign the form does not condition your treatment, payment, enrollment, or eligibility for benefits. However, there might be exceptions related to eligibility or enrollment determinations before being enrolled in a plan, and for health care provided solely for creating information for disclosure to a third party.
How can I revoke a previously given authorization?
You can revoke your authorization at any time by notifying UnitedHealthcare in writing. It's important to note that the revocation will not affect any actions taken based on your authorization before UnitedHealthcare received your revocation notice.
Who can I authorize to receive or disclose my health information?
You can authorize any individual or organization by mentioning their name and contact details on the form. This could include family members, healthcare providers, or legal representatives, depending on your specific needs and preferences.
What types of health information can be disclosed with this form?
The form allows for a broad range of health information to be disclosed, including drug and alcohol information, mental health details, HIV/AIDS status, psychotherapy notes, reproductive health, and sexually transmitted disease information, among others. You can specify the scope of information you're comfortable sharing.
For what purposes can my health information be used or disclosed?
Health information can be used or disclosed for various purposes, including but not limited to benefit management, administration of worker's compensation claims, claims administration/payment, administration of disability claims, employer mandated treatment or referral, and in response to a subpoena or other legal processes.
When does the authorization expire?
The authorization will expire on a specific date mentioned by you, or once a certain event you specify occurs. It's crucial to state a clear expiration date or event to ensure that your information is not used or disclosed beyond your preferences. Specific states may have additional requirements or provisions for the expiration of authorization.
Are there any special provisions for residents of specific states regarding the form?
Yes, there are state-specific provisions for Arizona, California, Georgia, Illinois, Indiana, Iowa, Minnesota, Oregon, Virginia, and Washington. These provisions can relate to how the request for medical records must be made, rights to receive a copy of the authorization form, expiration of the authorization, and requirements for witness signatures, among other details. It's important to review these provisions carefully to ensure compliance and to fully understand your rights and obligations under state law.
 All pertinent information UnitedHealthcare deems appropriate for the purpose checked below
All pertinent information UnitedHealthcare deems appropriate for the purpose checked below 
 Other (describe):
Other (describe):
 To allow the appropriate management of treatment, services, and/or coverage under the member’s benefit plan.
To allow the appropriate management of treatment, services, and/or coverage under the member’s benefit plan.